So many things affect your peripheral artery disease risk factors. And understanding your risk is critical, since preventing disease is far easier than treating the condition. Yet, somehow, many people fail to do so.
In fact, did you know that approximately one in five people over the age of 65 has peripheral arterial disease (PAD)? And that about 236 million people currently suffer from this condition, with cases on the rise? If that seems like a big risk to most older adults, there's a reason: it is! And that's because, as you get older, your risk for PAD increases dramatically. Here’s why.
PAD is a condition you develop when plaque builds up in your arteries. What is plaque? It’s a substance in your blood that’s made up of fat, cholesterol and other substances. When it sticks to the walls of your arteries, they ‘harden’—that’s called atherosclerosis, and atherosclerosis interferes with your blood’s ability to flow.
When it’s the blood flow to your legs that’s impacted by plaque, we call that condition PAD. And PAD can lead to leg pain and numbness. The hair on your legs may fall out; your skin color may change. You may find that cuts and scrapes take longer to heal; some wounds will no longer heal on their own when you have PAD.
But PAD symptoms aren’t just experienced in your legs. When you have PAD, your risk of heart attack, blood clots and stroke also increases. So does your chances of losing a limb to amputation.
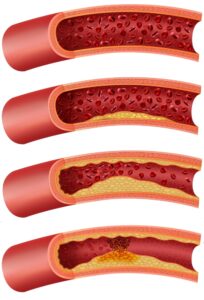
We don’t know the exact cause of this condition, and we learn new PAD risk factors regularly—in fact, in a poster presented at the National Kidney Foundation (NKF) 2024 Spring Clinical Meeting, we learned that symptoms of depression increase your risk for the disease. But aside from new developments such as this one, we know that PAD seems to begin when the inner layers of your arteries sustain damage due to a diet that’s high in fat and cholesterol; physical inactivity; a lifestyle that includes smoking; or having diabetes, high cholesterol and/or high blood pressure. Then, as your arteries begin to heal, plaque builds up along the walls.
Women and certain ethnicities also have higher risks for PAD. (Though we aren't sure exactly why.) And we know that too many people with asymptomatic PAD are at high risk for complications. Why is that the case?
Unfortunately, PAD can be hard to diagnose. That’s because many people with this condition don’t show any symptoms. Or, they experience symptoms like leg pain, numbness, and cramping, but confuse these problems for normal signs of aging, or for signs of other medical problems. That’s why it’s important to know all the PAD symptoms, which include: sores that don’t heal well; bluish skin color; skin that’s cold to the touch; problems with toenail growth; and, in men, erectile dysfunction.
A study from the International Journal of Environmental Research and Public Health now shows that migraines are a PAD risk factor. While they aren't sure why, it seems that migraine sufferers and PAD patients both have vascular abnormalities. For that reason, suffering from regular migraines could be considered an early PAD symptom. And, since PAD is often silent until damage is extensive, it's worth scheduling a diagnostic ultrasound if migraines are a regular problem from you.
Interestingly, the study found additional PAD risk factors. It noted that age, smoking, diabetes and hypertension all increase your risk for PAD. But it also added chronic kidney disease and asthma to the list of conditions that increase your PAD risk. Which means that, if you have any of these conditions, it's worth checking in with a PAD specialist.
That's also true if your BMI is on the higher side of optimal. Why is that the case? A study in the International Journal of General Medicine recently discovered that having a BMI below 25 decreased your PAD risk by 27%. Unfortunately, the opposite is true for those with a BMI that's higher than 25. In those cases, PAD risk was substantially higher. Meaning you should regularly check your arterial flow if your Body Mass Index is elevated.
Finally, a new study in Cardiovascular Research explored the link between PAD and psoriasis. Basically, uncontrolled psoriasis increased patients' risk for disease because skin-damaging inflammation could also impact your arteries and heart. As such, sticking with psoriasis medications could lower the risk for PAD complications, the study concludes.
If your vein specialist suspects you have PAD, you may need one or more of the following tests:
You may also need additional blood tests to check for related conditions like diabetes or high cholesterol.
If you are diagnosed with PAD early on, you may be able to control your symptoms with a series of lifestyle changes. At our Houston and Dallas area vein clinics, we also help PAD patients by using minimally invasive procedures. Some of the PAD treatment options we offer include Angioplasty, Stenting, and Atherectomy—the procedure we recommend for you will depend on the location of your blockages and the progression of your disease.
But want to know what they all have in common? These methods will almost always spare you from having major, open surgeries. Because of that fact, your recovery period will be drastically reduced. And you will likely be discharged from hospital on the same day of your procedure.
Before we come up with your treatment plan, however, we need to conduct diagnostic exams. And, in order to do that, we need to see you in the office. So, if you suspect PAD may be behind your leg cramps, or if you have any other PAD symptoms, schedule a consultation right awayschedule a consultation right awayschedule a consultation right away.

Scheduling
Please contact our dedicated specialists to schedule a consultation today.
2024 Texas Endovascular. All rights reserved. Website Design by Healthcare Success